Discover how we can help you find relief from posterior tibial tendon dysfunction.
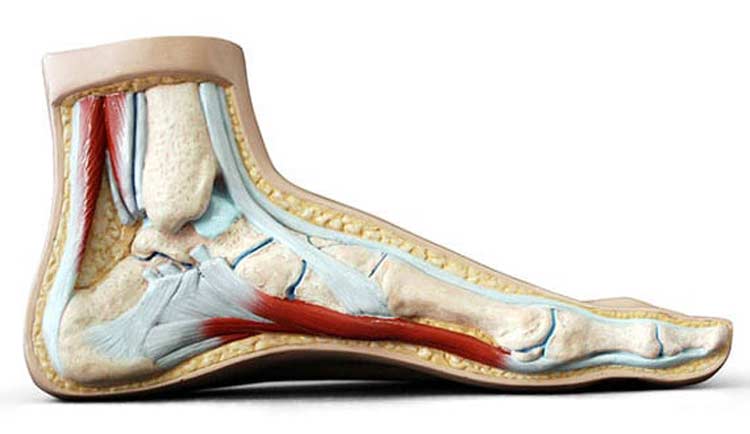
A significant supporting structure in the foot, the posterior tibial tendon plays an important role in walking and other foot movements. If this tendon is affected by an injury or some other issue, it’s referred to as posterior tibial tendon dysfunction (PTTD). PTTD is a condition in which changes to the posterior tibial tendon affect how the foot’s arch is supported.
- Patients with the condition usually notice a flattening of their arches, also known as flat feet.
- Patients often respond well to treatments for this progressive condition if it’s diagnosed and treated in the early stages.
Causes of Posterior Tibial Tendon Dysfunction
PTTD can occur in both feet, although it usually appears in one foot. It’s often referred to as “adult acquired flatfoot” since it’s the most common reason why flat feet develop later in life. The posterior tibial tendon may be slowly damaged by chronic overuse and pressure from certain foot and ankle movements. A sudden fall or some other type of acute injury may also cause the tendon to tear. When the tendon becomes damaged or inflamed, the foot’s arch will eventually collapse.
Risk Factors for PTTD
Anyone may injury the posterior tibial tendon. However, PTTD is often seen in women and adults over forty. Risk factors include having underlying health issues such as chronic hypertension or diabetes. Obesity is also a risk factor, as is participating in high-intensity sports.


PTTD Symptoms
Pain that’s felt along the back and inside of the foot and ankle is the most common symptom reported by patients with PTTD. There may also be noticeable swelling or inflammation in this area. Patients may also experience:
- Discomfort that gets worse with certain movements or activities
- Difficulty walking for long periods of time
- Numbness of general weakness of the foot and ankle
Podiatrist Evaluation and Diagnosis
A foot specialist will examine your foot and ankle. An evaluation typically involves looking for changes in the shape of the foot and signs of visible swelling. Normally, when the toes are viewed from the back of the heel, only four of them are visible. With PTTD, all five toes may be visible from this view.
Other than a foot examination, diagnosis usually involves asking the patient to attempt to stand on one leg and raise their heel. Patients with a damaged posterior tibial tendon cannot perform this action. X-rays, CT scans, and MRIs may also be done to determine the extent of the damage to the tendon and to rule out the possibility of arthritis, which can produce similar symptoms.
Non-Surgical Treatments
Patients with PTTD often notice a gradual reduction in discomfort with non-surgical treatments. One of the first suggestions usually made is for patients to modify their activities to take direct pressure off of the affected ankle. For instance, instead of going for a daily run, a patient may use an elliptical machine to work similar muscle groups. When the pain is initially felt in the around the ankle, applying ice 3-4 times a day in 15-20 minute intervals may ease tendon swelling. Because it takes time for the posterior tibial tendon to heal, it may take 3-6 months to see results from any of the following treatment options:
- Immobilization with a leg cast or walking boot for about 6-8 weeks
- Anti-inflammation medications
- Steroid injections directly into the posterior tibial tendon
- Physical therapy exercises specifically for feet and ankles
- Over-the-counter or prescription orthotics
Surgery for PTTD
Surgery is usually only an option if conservative treatments aren’t providing sufficient relief after six months or so. The specific procedure recommended will depend on the extent of the damage to the tendon.
Gastrocnemius recession is a procedure that involves lengthening of the Achilles Tendon. It can prevent arches from falling again. However, patients may feel some weakness while climbing stairs.
When PTTD is mild and the shape of the foot hasn’t changed, a tenosynovectomy may be done. During the procedure, inflamed tissue around the posterior tibial tendon is removed.
With a tendon transfer, the diseased posterior tibial tendon is removed. It’s replaced with another tendon from the foot. In some instances, the transferred tendon may be placed alongside the posterior tibial tendon.
If surgery is necessary, the amount of time required for a full recovery will vary based on the severity of the condition. Some patients will get back to their normal activity level within several months while others may need a full year to recover completely. Since overuse and stress are the most common causes of PTTD, making an effort to avoid repetitious foot movements, maintaining a healthy diet, keeping weight in check, and doing a proper stretch before engaging in sports-related activities can help prevent damage to the posterior tibial tendon.

