Discover how we can help you find relief from Haglund’s deformity.
Haglund’s deformity manifests as a bony bump at the back side of the heel. As the bony protrusion rubs against shoes, it irritates the soft tissue around the Achilles tendon.
- This irritation can lead to bursitis, which is inflammation of the bursa, a fluid sac located between bone and tendon.
- With inflammation, there is a tendency for calcium to accumulate in the heel, which makes the deformity larger and more painful.
Causes
Certain factors increase the likelihood a person will develop Haglund’s deformity. One of them is inherited foot structure. Those with a high-arched foot or a tight Achilles tendon develop the deformity more often. Also prone to Haglund’s are those who tend to walk on the outer edge of the heel.
Common among women who wear pump-style shoes, the deformity has the nickname of pump bump because these type shoes allow friction between the bone and the shoe. Other footwear also contributes to Haglund’s. Shoes with a rigid back, including men’s dress shoes and ice skates, can lead to irritation.
Symptoms
One or both feet may be affected by the deformity. Symptoms include a noticeable bony bump behind the heel, swelling in that area and redness near any inflamed area. Pain is a big indication of Haglund’s and is noticeable where the Achilles tendon is attached to the heel. Some people also develop painful blisters on the heel due to the friction of their shoes rubbing the bump deformity.


Diagnosing the Problem
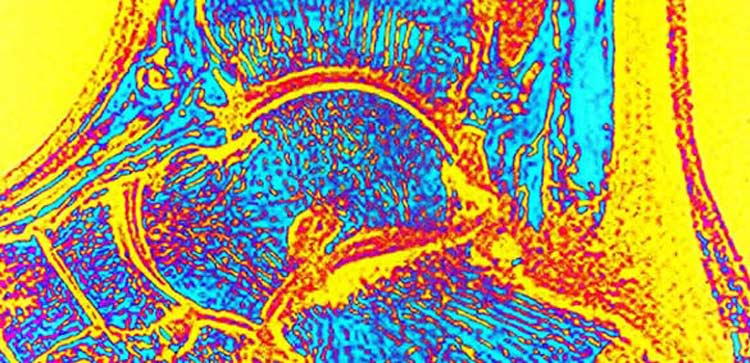
Because its symptoms are similar to other foot problems, such as Achilles tendonitis, diagnosing Haglund’s deformity can be challenging. Sometimes a podiatrist can diagnose it based on how the heel looks. Other times the doctor orders an X-ray, MRI or ultrasound to look closer at the foot structure in order to make an accurate diagnosis.
Non-Invasive Treatment
Several non-surgical treatment options aim to reduce the swelling of the bursa, which can lessen pain. Non-surgical treatment focuses on either the shoes or the body.
The Shoes
Heel lifts work to lessen pressure on the heel and work well for people with high arches. To reduce irritation while walking, heel pads positioned inside the shoe’s cushion can help. Another way to minimize irritation is to modify the type of shoes worn to include those with no back or a soft back. Podiatrists may recommend customized arch supports to control foot motion.
The Body
Patients with a tight heel cord benefit from stretching exercises that relieve tension in the Achilles tendon. Physical therapy is beneficial for all Haglund’s suffers, and soft tissue massage may help. Patients can put ice on inflamed areas for about 20 minutes to reduce pain and swelling. Doctors sometimes use a cast to keep the foot immobile. Oral anti-inflammatory medicine is typically recommended for pain and inflammation.
Surgical Options
Because non-surgical treatment does not get rid of the bony deformity and may not provide a patient the relief they need, a podiatrist may suggest surgery. It is also an option when the bony bump is too prominent or there is Achilles tendon degeneration, which includes a small risk of the tendon rupturing.
For surgery, patients are under anesthesia or given a nerve block around the knee to numb the leg. To remove the bony protrusion, the surgeon makes an incision at the heel next to the Achilles tendon. Typically, the incision is on the inside of the heel. For a degenerative Achilles tendon, the doctor usually makes an incision in the midline. Some tendons are repairable. The surgeon removes the bony bump and the tendon that is not repairable. Sometimes the surgeon transfers a tendon to the heel to replace part of the damaged Achilles.
Recovery
When surgery is for bone removal only, the patient wears a splint for two weeks after the procedure. The patient puts no weight on the affected heel for two weeks. They are allowed some weight-bearing after that, and after a few days, can bear full weight on the foot. For procedures that involve tendon repair or removal, weight bearing is often delayed. Patients get a boot that has a heel lift, and they likely start physical therapy two weeks after surgery. While going through therapy, the patient progresses to a point that the heel lift is removed from the boot, and eventually, the boot is no longer needed.

